 I'm back!
I'm back!Jason Witten suffered of the Dallas Cowboys an unusual injury - a lacerated spleen - in an exhibition game against the Oakland Raiders when he was hit by Rolando McClain in what looked like a relatively clean, legal and solid tackle.
Between the incident and until he gets examined again, he's not allowed to engage in any form of physical contact, including running drills, working out or practicing. Cowboys' coach Jason Garrett stated "he has to stay very idle." He's played through multiple injuries including what was likely a painful rib fracture in the past.
What's the difference now? In short, the spleen is an organ you don't want to mess with.
Let's start by examining the diagnosis and management of a spleen laceration.
Presentation: Typically, damage to the spleen presents due to blunt trauma to the abdomen or left flank. Most commonly this type of injury is seen in motor vehicle accidents, but can also occur in high impact sports or assault.
It makes sense that the patient would complain of left-sided pain, and sometimes left shoulder pain. The left shoulder pain is part of "Kehr's sign" which is a "classical" (anyone know sensitivity/specificity?) presentation of intraabdominal bleeding that causes left shoulder pain when the legs are elevated. This pattern occurs because irritation of the diaphragm (by blood in the abdomen or trauma) causes referred pain into the shoulder.
The patient will usually also complain of abdominal pain or have other signs of peritonitis (or intraabdominal bleeding or inflammation), but all of the above symptoms are not sensitive or specific for splenic injury. Combining clues from the history and physical should make the physician suspicious of a possible splenic injury.
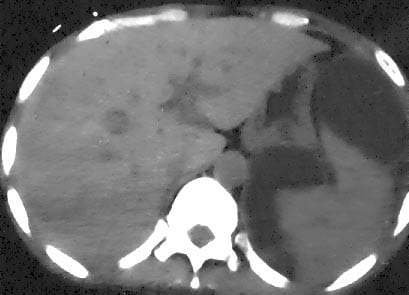 |
| Figure 1: A splenic injury causing bleeding in the abdomen and a "mass effect" pushing the spleen towards the back Credit: eMedicine |
In a stable patient, a CT scan with contrast would be done to effectively rule in or rule out a splenic injury, and also to grade its severity which is important for management.
Figure 1 (from eMedicine) shows a CT visualizing the spleen on the patient's left (your right) side. The dark material around the spleen is blood surrounding it, pushing it into a bizarre shape and out of place.
Treatment: Management of a splenic injury is typically either surgery or watchful waiting to ensure it heals on its own. Whether surgery or medical management is chosen depends on a number of factors including:
- hemodynamic stability -- i.e. is the patient rapidly losing blood or in shock?
- Grade on the American Association for the Surgery of Trauma Spleen Injury Scale - this predicts how likely non-surgical management will suffice in treating the injured spleen. For example, grade I injuries have a 5% chance of failing and needing surgery while 40% of grade IV injuries will require surgery.
- the amount of abdominal bleeding seen on CT scan
In total, non-operative management of spleen injuries has a failure rate of 10-15%.
More recently, there have been some non-invasive procedures utilized to increase the likelihood non-surgical management will succeed but I won't go into that right now.
What do you do while you wait? What happens when it fails?
The patient would have to be closely monitored for a number of days under close medical care, often admitted to hospital. They are checked for signs of blood loss and staff ensure their vitals remain stable. One large trial found 86% of cases of non-operative management failed within 96 hours. Needless to say, he or she should not be playing football or working out.
Failure of observation can result in a "delayed splenic rupture" which can result in massive blood loss and the patient possibly going into shock.
While we don't know the details of Witten's injury or the severity of it, it's fortunate he hasn't required surgery. Despite things looking up so far, he's not out of the woods just yet and he'll have to see what his doctors say in the coming days when they re-evaluate him. In fact, many patients (of course depending on the injury) are advised to not resume high-risk activities for a period of three months. I should mention though that this recommendation is based on expert opinion and the hypothesis the spleen could easily re-injure.
Sources:
UpToDate
Tintinalli's Emergency Medicine, 7th edition





