In Week 10 against the Tampa Bay Buccaneers, QB Matt Schaub of the Houston Texans sustained a Lisfranc fracture. It's not a very common injury, and is actually often missed.
 Firstly, the loose term of "Lisfranc joint" can be applied to the connection between the metatarsals (most proximal long bones of the foot; analogous to the metacarpals that are the bones in the palm of the hand) and cuneiforms (analogous to the carpals, or wristbones, of the hand).
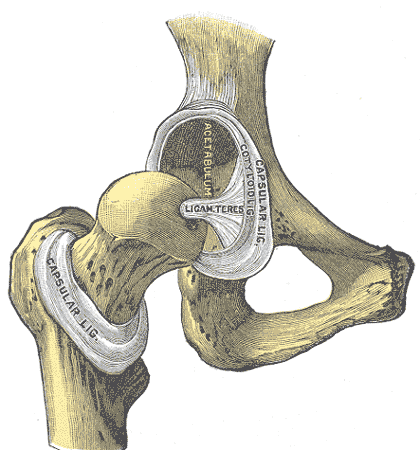
Firstly, the loose term of "Lisfranc joint" can be applied to the connection between the metatarsals (most proximal long bones of the foot; analogous to the metacarpals that are the bones in the palm of the hand) and cuneiforms (analogous to the carpals, or wristbones, of the hand).The Lisfranc ligament is what connects this joint and goes from the first (medial) cuneiform) to the second metatarsal. No other ligaments connect the cuneiforms and the metatarsals to each other.
Clear as mud?
How does it occur? Intuitively, since this ligament is all that connects the metatarsals and cuneiforms together, it is prone to injury. This usually occurs either by a direct blow to the joint itself or an increased load to the joint (think of when you're on your toes) accompanied by a rotational force. An example could be of a horseback rider falling while their foot is stuck in the stirrup.
What is the injury? There is a spectrum of injuries that can happen to the Lisfranc ligament.
- Grade I sprain: Pain at joint, no swelling
- Grade II sprain: Increased paint at joint, some swelling, slight laxity but no instability
- Grade III sprain: Complete disruption of ligament; could include a fracture dislocation (this is what Schaub sustained). Any injury of above Grade III doesn't affect prognosis.
How is it diagnosed? A good history of the mechanism of injury should raise suspicion of its possibility. It may present as simply as swelling and the inability to weight bear. The physician should palpate the joints within the foot and do his/her best to localize tenderness.
In terms of the fracture-dislocation, it can be diagnosed by X-ray which would show disruption of the normal alignment of the joint and possibly a bone chip caused by the ligament breaking off from one end.
How is it treated? Most sprains that are stable and not displaced can be treated medically with analgesia and rehabilitation. In athletes, there is a low threshold for treating it surgically given that no surgery can lead to instability, severe pain and damage in the future. The surgery performed is to fixate the joint with screws or wires. In terms of healing, the patient needs to wear a cast and cannot weight-bear for six weeks as the joint heals. Activity and rehabilitation can be increased as symptoms abate.
Sources:
eMedicine
American Association of Family Physicians